A NEW ECONOMIC LENS FOR B.C. HEALTH CARE (2023)
Issue
Innovation and technological advancements are extremely fast paced, but B.C.’s healthcare system has the opportunity to catch up. B.C. and Canada has an aging population. Acute intervention, which accounts for 80% of publicly funded dollars but serves less than 20% of the population, will be more costly in the future[1]. Now is the time for innovative strides in the public health care system by implementing a chronic care management system that includes the physician and nurses, patients and their social and community support systems, and technologically innovative organizations.
Hospitals also remain fundamental to the healthcare system but are not funded to ensure healthcare delivery is equitable.
Background
A healthy population is an efficient and productive population. Cardiovascular disease, stroke, diabetes, and cancer are among the main diseases that affect Canadians[2]. These diseases manifest over time and need to be appropriately managed in an efficient way before they become detrimental to our economic production capacity. A healthier population now also means that down the road – with the current trend of an aging population in Canada – society will observe less costs in the healthcare system.
As it stands, cardiovascular diseases, stroke, diabetes, and cancer are managed by acute intervention (via surgery). Acute intervention accounts for 80% of the money invested by the public and helps 20% of the population, many times when it is too late. This area of intervention is handled solely by doctors, and there is we are seeing a declining trend in e in the total number of patients that general practitioners in B.C. see day-to-day[3]. At this point, doctors are stressed, overworked, and in need of assistance.
India has an enterprise known as Apollo Hospitals Enterprise Ltd that delivers a single point of access that provides the care for and management of chronic diseases. It includes a pharmacy, physicians, dental physicians, physiotherapy, and telemedicine[4]. This innovative hospital also provides patients with access to healthcare in the form of including community and social networks, which can be your priest, your family, and your friends. By including all of these aspects in one area, patients can consult with many experts and it will alleviate the pressures on the primary care provider, the Family Physician.
Working with medical professionals, Apollo has endeavoured to advocate for a system that would alleviate the pressure on the current healthcare model. In addition to the GP and nurses within the current acute intervention model (i.e. hospitals), they have many healthcare providers working in tangent to ensure that patients have well-rounded support systems. Apollo envisions a reform where care is delivered in a continuum. The patient is empowered to involve their social network with other professionals in the healthcare industry.
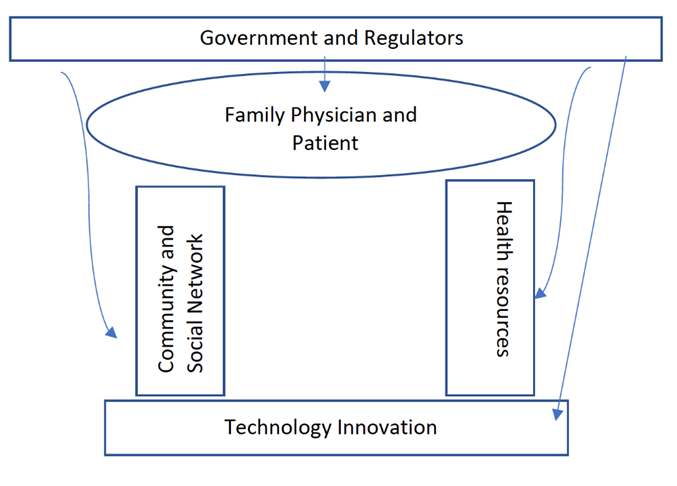
In this innovative approach, the GP and patient would be central to the chronic care management/primary care system. The government would work with regulators to provide funding, research, and incentives; they would also ensure accountability. A pillar supporting the GP and patient would be the resources – this would include many NGOs, other care deliverers, and the local healthcare regulators (i.e. Fraser Health). The other pillar of support would be the community and social network of the patient.
Finally, there would be the technology industry providing innovative approaches to care delivery. The system is illustrated by figure 1 below. The arrows indicate that government and regulatory bodies provide funding and incentives to the various actors within the system. At the same time, feedback and monitoring must be persistent in the entire system and so the program can adapt to changing circumstances. The system and its actors would work collaboratively and congruently to ensure that optimal care is delivered to the patient.
Figure 1 The Hierarchy of Health
Actions We Can Take Now And Why Health Care Matters To Business:
The failure of our system to adapt to the changing needs of British Columbian’s has left a very expensive health-care system that delivers mediocre results, as stated by the physicians and healthcare professionals we worked with in developing this policy. COVID-19 has made it evident that healthy communities lead to economic prosperity, and that unhealthy or unwillingness for individuals to adequately take care of themselves creates economic uncertainty. British Columbians should have a health-care system that is truly worthy of their confidence and trust. There are five clear steps that could be taken to achieve this:
- Integration and Innovation
Health-care stakeholders in B.C. still function in silos. Hospitals, primary care, social care, home care and long-term care all function as entities unto themselves. There is poor information sharing and a general failure to serve common patients in a coordinated way. Ensuring that the patient is at the centre — regardless of where or by whom they are being served — will lead to better, safer, more effective and less expensive care. Investments in information systems will be key to the success of these efforts. If investments in technology and information systems are made this will benefit workers to ensure they have the integrated health care knowledge that they need in an expedient pathway - taking limited time away from the workplace. - Enhanced Accountability
Those who provide healthcare to British Columbians, there needs to be greater accountability and models focused on outcomes rather than outputs. Quality and effectiveness should be rewarded rather than the amount of service provided. Alignment of professional, patient and system goals would ensure that everyone is pulling their oars in the same direction. Improving accountability would provide better peace of mind for people to return to work and provide business owners peace of mind that their employees are being given outcome orientated treatments. - Broaden the Definition of Comprehensiveness
Many factors influence the health of British Columbians in addition to doctors’ care and hospitals. So why does our “universal” health-care system limit its coverage to doctors’ and hospital services? A plan that seeks health equity would distribute its public investment across a broader range of services. A push for universal Pharmacare, for example, is currently under way in Canada. Better integration of health and social services would also serve to address more effectively the social determinants of health. - Bold leadership
Bold leadership from both government and the health sectors are is essential to bridge the gaps and break down the barriers that have entrenched the status quo. British Columbians need to accept that seeking improvements and change does not mean sacrificing the noble ideals on which our system was founded. On the contrary, we must change to honour and maintain those ideals. Our leaders should not be afraid to set aspirational goals.[5] - Hospital Investments
The World Health Organization indicates that the minimum hospital beds a geographical area should have is 1 bed per 1000 citizens. Below is a comprising of hospital beds versus population (2021 census data).
There are many hospitals throughout the lower mainland that service the entire Metro Vancouver region.
- SMH 634 beds vs population 568,320
- Abbotsford – 300 beds vs population 153,524
- Royal Columbian Hospital (New Westminster) - 490 beds vs population 78,916
- Langley Memorial - 188 beds vs population 166,356 (City and Township)
- Peace Arch (White Rock) - 146 beds vs population 21,939
- Burnaby Hospital - 314 vs population 249,125
- Vancouver General Hospital and Health Sciences Centre - 1300 acute; 6,700 residential; 80 rehabilitation; 900 assisted living/respite beds
- St. Paul’s Hospital, Mount Saint Joseph Hospital - 2,000 acute; 6,700 residential; 270 rehabilitation; 900 assisted living/respite beds
The Fraser Health Authority denotes Surrey Memorial Hospital as a regional hospital[6], however, it does not have the facilities required to treat three of the leading causes of sudden death: heart attack; stroke and trauma. Those patients must be transported to Royal Columbian Hospital (RCH). Unfortunately, if there is a natural disaster that prevents access to RCH, there is no hospital south of the Fraser River that can treat heart attacks, strokes, or certain types of trauma.
FHA and therefore Surrey have historically received less per capita than Vancouver for health care. A review of the 2020/21 audited statements of FHA and Vancouver Coastal show that: FHA received $2,229 per person. Vancouver Coastal received $3,033.
BC Ambulance statistics for 2021 show that 1376 patients were transferred from SMH to other cities for care. The top three reasons were heart, stroke, and pediatric specialty care.
The new Surrey hospital is projected to have 168 beds bringing Surrey's total beds up to 802. Although this satisfies the WHO's minimum beds per 1000 persons in a geographical area, it still fails to satisfy the needs of the region.
The new hospital will have: 5 operating rooms; 4 procedure rooms; an emergency room with 55 treatment spaces; virtual care options; 3 CT scanners; 2 MRI machines; a pharmacy; a laboratory, and; academic spaces. All these services with an additional cancer research facility are expected in the $1.72 billion hospital.
As it stands, there is no emergency plan that addresses how residents living south of the Fraser River will access these lifesaving services in the event of an earthquake or natural disaster that affects bridge and tunnel crossings.
The provincial government has made some significant investments in healthcare as it relates to acute care, especially in budget 2023[7]. The federal government has also provided more funding for healthcare[8]. These investments must be made in aspects of healthcare that is being asked for by our medical professionals.
THE CHAMBER RECOMMENDS
That the Provincial and Federal Governments:
- Invest in greater hospital capacities in the areas that will see high levels of population growth.
- Develop an emergency plan that addresses how residents will receive care given a large-scale natural disaster.
- Close the gap in chronic care and empower the patient to manage their health by utilizing self-management, behaviour modification, and lifestyle, which includes: Family Physician, nurses, the patient, community and social support systems, and technologically innovative organizations.
[2] https://www.canada.ca/en/public-health/services/publications/healthy-living/how-healthy-canadians.html
[3] https://vancouversun.com/news/local-news/number-of-b-c-doctors-growing-but-work-life-balance-means-fewer-patient-visits-worsening-access
