B.C.‘S HEALTH SYSTEM – TIME TO EVALUATE AND REVIVE (2023)
Issue
The medical system in British Columbia and across the country is broken! We are at a crossroads in healthcare where we have to find solutions. The time to point fingers is over. We need to look at the system from the top down and re-connect the community voice with community health.
Background
In a province as diverse, wealthy and educated as British Columbia there is no excuse that lack of health care impacts quality of life. Provinces are the gatekeepers to health and if the pandemic proved anything it is that the provinces and the federal government can put politics aside. We saw, despite the controversies, that provinces and the federal government can hear the voices, work together and find solutions.
In 1961 Premier Tommy Douglas announced his plan for universal publicly funded medical insurance coverage (Medicare) in Saskatchewan. On July 1st, 1968 the Medical Care Insurance Act came into effect in Canada. By 1971 all provinces had established comprehensive medical insurance plans that met the federal criteria for funding eligibility.
Universal access to medical services is a source of pride for Canadians and yet across the country we daily read about the failures of the system to provide the health care British Columbians and Canadians need.
We need to stop the steady decline of our health system. Solving the crisis requires more than just funding – it requires an in depth evaluation of the organization and systems with the objective of ensuring British Columbians and Canadians have access to truly universal, equitable health care.
We are in a crisis, that has been a very long time in the making. We cannot afford to continue to treat the symptoms while ignoring the disease.
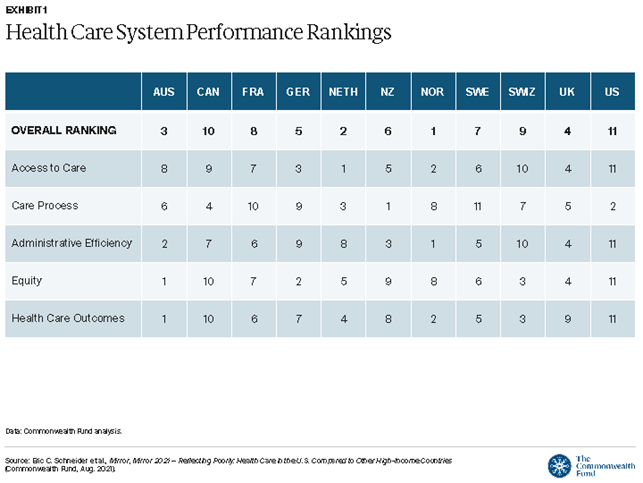
In the most recent Commonwealth Fund Report 2021[1] Canada ranked #10 out of 11 countries and reports dating back to 2010 have showed a steady decline with Canada in the bottom 2 countries for health care consistently.[2] Scoring in the bottom for Health Care Outcomes, Equity and Access to Care but 4th in the Care Process. Once in care our health care professionals go above and beyond for patients. So how do we ensure that access to care is universal and equitable? By stepping back and looking at our health care system from 50,000 feet. Not picking at the individual details, not pointing fingers or placing blame. Looking at the countries that are having success and putting best practices into place in British Columbia. It is time for a different tactic. “The definition of insanity is doing the same thing over and over and expecting different results.” -Albert Einstein
As more and more British Columbians struggle to access family doctors, diagnostics, home care, and maternity we need government, health authorities, service providers and communities to step back and look at the overall system. CBC.[3] reported that 59% of B.C. respondents to an Angus Reid poll found it difficult to access a family doctor and that 36% do not have a family doctor despite wanting one. This equates to almost a million residents without primary care.
We see rotating and/or permanent closures to hospitals, clinics, maternity, diagnostic services, removal of low acuity procedures in remote communities, lack of access to timely care/procedures and so much more. Health care professionals seek more than just financial incentives – they are seeking quality of life, better working conditions, work life balance and the support to do their jobs. Imagine bringing team based centres/ labs/small surgical centres back to smaller communities providing care and the opportunity for residents of larger centres to travel for quicker service providing those communities with economic opportunities. Turn to communities across B.C. to enhance services, provide more at home/in community care and relieve some of the burden on larger centres while providing health care professionals opportunities for affordable housing in family friendly communities.
The centralization of health care through 6 regional health authorities isn’t working, particularly for rural and remote communities. In the Northern Health region Municipalities[4], Chambers[5][6] and the Resource Municipalities Coalition[7] have all called for audits of the health authority. Centralization isn’t working – the voice of the community once represented by a local hospital board with a broad community base has been eliminated and replaced with individual complaint driven processes. Where once communities had a role and partnership with government on healthcare and were resources to identify trends and gaps, they have been effectively silenced with no direct engagement opportunities. This disconnection of the community voice and the increased means (social media) to complain to a wider audience creates extremism and unrest as we have seen throughout the pandemic. Health authorities spend less time on actually finding solutions and providing health services and more time defending their actions or inaction. Health Authorities are in protectionism & survival mode. We need to replace that with growth, efficiency, sustainability and caring for both the patient and the health care provider.
“The best health systems in the world depend on four principal factors: barrier-free universal coverage, significant commitments to primary care, few administrative burdens and an investment in social service – nutrition, education, childcare, housing, transportation, community safety and worker benefits – to help keep people from the system itself.” – Kirk LaPointe[8]
We require a high-level holistic overview of the British Columbia health system – what parts of the system work well and where are we broken with a lens on team care in communities that is universal across the province and inclusive of rural and remote communities, indigenous communities and marginalized groups (Seniors, GLBTQ2S, Racial/Cultural Minorities, Persons with Impairments).
THE CHAMBER RECOMMENDS
That the Provincial Government:
- In partnership with the Federal Government convene an independent panel to review those countries that rank highest in access and health outcomes (Norway, Netherlands, Australia) to apply best practices to B.C. and Provincial Health Systems and make the findings of the panel public.
- Convene an independent panel to review the Regional Health Authorities structure and effectiveness to ensure they are connected and accountable to the communities they serve.
